Paracetamol is one of the most commonly used medications in households worldwide. Whether it’s for fever, headache, or mild body aches, this go-to drug is almost always within reach. But how much do we really know about this familiar medicine?
Let’s explore everything you should know about Paracetamol — including how it works, correct dosage, who can safely use it, and when to avoid it.

What Is Paracetamol?
Paracetamol belongs to a group of drugs known as antipyretics (fever reducers) and analgesics (pain relievers). It is often used for treating:
-
Fever
-
Headache
-
Toothache
-
Muscle pain
-
Mild arthritis pain
How Does Paracetamol Work?
When you experience fever or pain, your body releases certain chemicals called prostaglandins, which increase inflammation, pain, and body temperature. Paracetamol works by blocking the enzymes that produce these prostaglandins, thereby reducing discomfort.
Additionally, it acts on the brain through a pathway known as the descending serotonergic pathway, helping to relieve pain centrally.
So, in simple terms — Paracetamol reduces pain and fever by working at the chemical level in your body and brain.
Recommended Dosage of Paracetamol
For Adults:
-
Dosage: 500 mg to 1000 mg
-
Frequency: Every 6 to 8 hours as needed
-
Minimum gap: 4 hours between doses
-
Maximum daily limit: 4000 mg (4g)
⚠️ Taking more than the recommended dose can cause serious liver damage.
For Children:

-
Dosage depends on body weight
-
Must be prescribed by a pediatrician
-
Never self-medicate or guess the dose
It’s safe to take Paracetamol with or without food.
Who Can Safely Take Paracetamol?
Paracetamol is generally considered safe for:
-
Children (with pediatrician guidance)
-
Adults
-
Elderly
-
Pregnant women
-
Breastfeeding mothers
Its safety profile makes it one of the few over-the-counter medicines used across age groups.
Who Should Avoid or Be Cautious With Paracetamol?

Even though it’s widely used, there are certain groups who need to be cautious:
-
People with liver or kidney disease
-
People who consume alcohol regularly
-
Those with an allergy to Paracetamol
-
Patients on medications like Warfarin (blood thinners), epilepsy drugs, or tuberculosis treatment
These individuals should only take Paracetamol after consulting a healthcare provider.
Possible Side Effects of Paracetamol
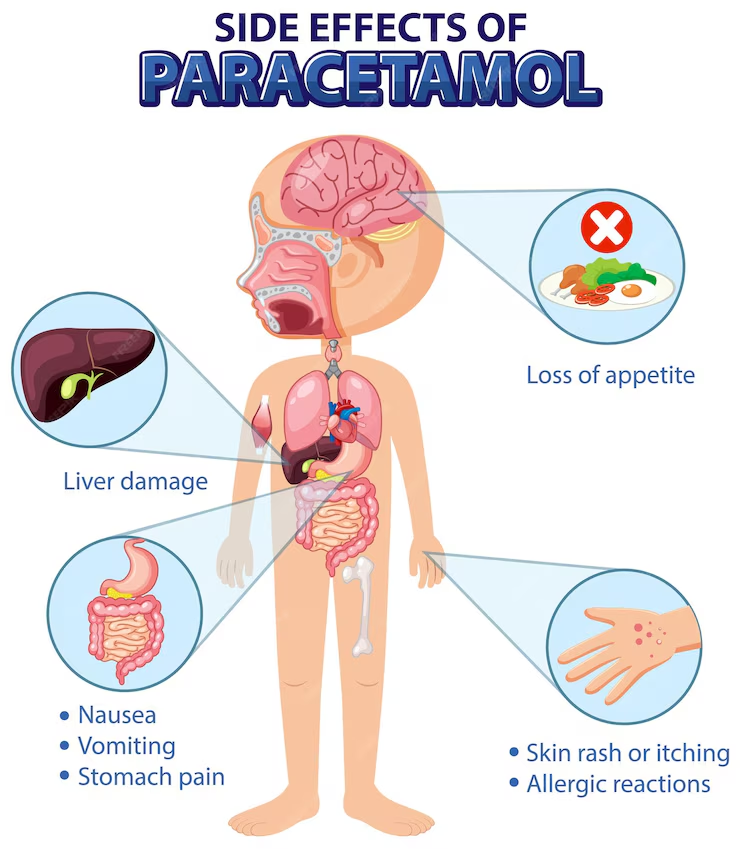
While Paracetamol is usually well-tolerated, overuse or misuse can lead to:
-
Liver damage
-
Kidney issues
-
Gastrointestinal bleeding
-
Allergic reactions (rash, itching, swelling)
-
Paracetamol toxicity/poisoning
What is Paracetamol Poisoning?
Paracetamol poisoning occurs when too much of the medicine is taken — either all at once or over a short period. It can lead to acute liver failure, which can be life-threatening if not treated promptly.
This is especially dangerous for children. Even 500 mg can be toxic for small infants.
Common signs of overdose or poisoning:
-
Nausea, vomiting
-
Stomach pain
-
Confusion or drowsiness
-
Jaundice (yellowing of eyes/skin)
Signs of a Drug Allergy (Serious Reactions)
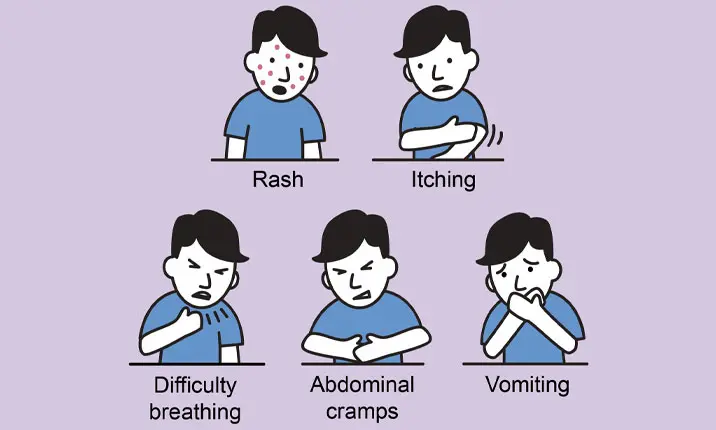
Some people may experience severe allergic reactions to Paracetamol. These can be life-threatening and require immediate medical attention.
Symptoms include:
-
Skin rashes or hives
-
Difficulty breathing
-
Chest tightness
-
Swelling of lips, tongue, or face
🚨 If you notice any of these symptoms, seek emergency care immediately.
Top 10 Essential Things to Remember About Paracetamol
-
Don’t double the dose if fever or pain doesn’t subside. Wait at least 4 hours before taking another dose or try a different medicine recommended by a doctor.
-
If pain relief isn’t achieved, consult a doctor instead of repeatedly taking Paracetamol. A different painkiller may be more effective.
-
Avoid combining Paracetamol with alcohol. This combination increases the risk of severe liver damage.
-
Check for drug interactions. If you’re on TB treatment, epilepsy medication, or blood thinners, talk to your doctor before taking Paracetamol.
-
Avoid taking multiple medications with hidden Paracetamol. Many cold and flu medications already contain Paracetamol. Read labels to prevent accidental overdose.
-
Pregnant or breastfeeding women should take only the minimum effective dose for the shortest duration possible.
-
Never give Paracetamol to children without a doctor’s advice. Dosing must be weight-specific.
-
Always maintain a 4-hour gap between doses. An 8-hour gap is even safer, especially for long-term use.
-
Don’t ignore allergic reactions. Symptoms like rashes or breathing difficulty should not be overlooked.
-
Use non-drug remedies first, like rest, hydration, or cold compresses. Only rely on medicine when necessary.
Summary Table
| Topic | Key Info |
|---|---|
| Drug Class | Analgesic & Antipyretic |
| Common Uses | Fever, headache, mild pain |
| Adult Dosage | 500–1000 mg every 6–8 hours; max 4000 mg/day |
| Child Dosage | Weight-based; only on pediatrician’s advice |
| Safe For | Adults, elderly, pregnant/lactating women, kids (with care) |
| Avoid If | Liver/kidney disease, alcohol use, allergy, drug interactions |
| Main Side Effects | Liver/kidney injury, GI bleeding, allergic reactions |
| Paracetamol Poisoning | Overdose leads to liver failure |
| Allergy Signs | Rashes, breathing issues, facial swelling |
| Pro Tip | Always check combo drugs to avoid accidental overdose |
Final Thought
Paracetamol may seem harmless, but like any medicine, it must be used responsibly. The key to safe usage lies in correct dosage, timing, and being aware of underlying health conditions or other medications.
When in doubt, consult your doctor — especially for children, elderly, or if you’re already on other medications. Don’t self-medicate beyond recommended limits, and always keep it out of reach of children.