As a critical care physician, managing patients on and off ventilators is part of daily practice. However, for most families, the concept of a ventilator is unfamiliar and deeply distressing. Questions like “What is a ventilator?”, “Why is my loved one on it?”, and “Will they recover?” are common.
This article will walk you through what a ventilator is, when it’s used, what the patient experiences, and what families should understand during this critical time.
What Is a Ventilator?

A Simple Explanation
A ventilator is a machine designed to assist or completely take over the breathing process for patients who are unable to breathe adequately on their own. It’s also called a “breathing machine” because it pushes air into the lungs and then pulls it out, mimicking natural breathing.
Just like our lungs inhale oxygen and exhale carbon dioxide, the ventilator does the same – but mechanically, and with high precision.
How Is a Patient Put on a Ventilator?
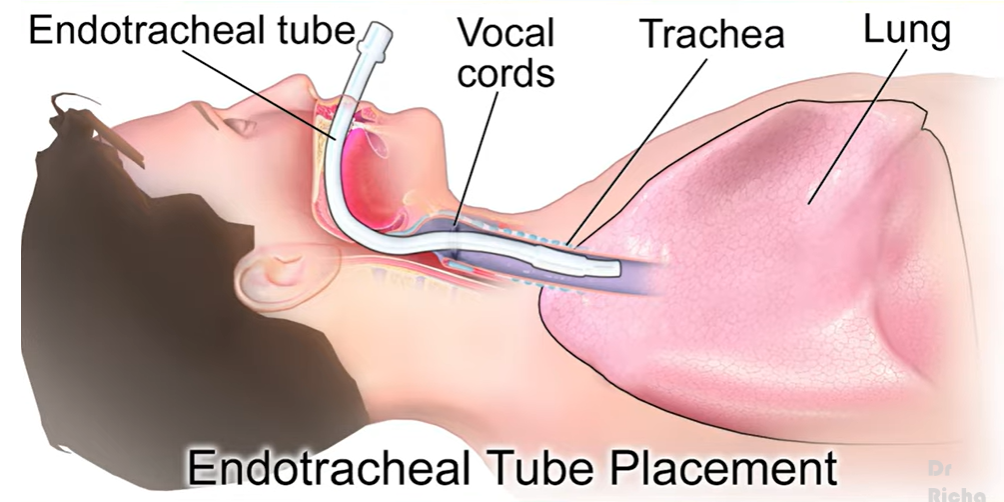
To place a patient on a ventilator, a tube is inserted through the mouth or nose down into the windpipe (trachea). This process is known as intubation. Once the tube is securely in place, it’s connected to the ventilator machine, which then starts supplying oxygen and helping the patient breathe.
Is Intubation Painful?
Yes, inserting the tube can be uncomfortable. That’s why patients are usually sedated (kept unconscious or in a sleep-like state) before the procedure. This ensures they don’t feel pain or distress while the ventilator is in use.
When Do Doctors Use a Ventilator?
Ventilators are never the first option. They are used only when absolutely necessary – typically when a patient’s lungs are too weak or damaged to breathe properly.
Common Conditions Requiring Ventilator Support
-
Severe lung infections like pneumonia
-
Asthma attacks that do not respond to treatment
-
Chronic lung diseases like COPD
-
Major surgeries requiring general anesthesia
-
Accidents causing major trauma or blood loss
-
Brain injuries or unconsciousness where breathing control is impaired
-
COVID-19 or other severe respiratory illnesses
-
Neurological diseases causing breathing weakness
If a doctor recommends a ventilator, it usually means all other non-invasive methods have failed, and mechanical support is now critical to save the patient’s life.

Is It True That Doctors Put Patients on Ventilators to Make Money?
This is a myth – and a dangerous one.
No ethical doctor ever puts a patient on a ventilator for monetary reasons. The decision is based solely on medical necessity. In fact, ventilators are costly not just because of the machine, but due to the specialized care involved:
-
Continuous monitoring by ICU staff
-
Expensive medications
-
Constant supervision by nurses and respiratory therapists
Ventilation is recommended only when it can potentially save the patient’s life.
Can Patients Recover After Being on a Ventilator?
Absolutely, yes. Many patients successfully come off ventilators, recover, and return to their normal lives.
However, the outcome depends on several factors:
Better Recovery Chances:
-
Young age
-
Reversible illness (e.g., pneumonia)
-
Single organ failure
-
Short duration on ventilator
Poor Recovery Prognosis:
-
Advanced-stage cancer
-
Multiple organ failure
-
Old age with frailty
-
Prolonged ICU stay due to chronic conditions
The key point is that many patients do recover, and it is wrong to assume that being on a ventilator is a death sentence.
Why Is the Patient Not Responding While on Ventilator?
This is another common concern from families. Often, the patient may appear unresponsive or unconscious while on a ventilator. That’s because sedation is used to keep them comfortable and synchronized with the machine.
Why Sedation?
When a patient breathes slightly on their own while also receiving mechanical breaths from the ventilator, it can cause a mismatch. Sedatives help the patient adapt better to the ventilator, ensuring healing happens faster and safely.
Can a Ventilated Patient Talk or Eat?
Talking:
No. The breathing tube passes through the vocal cords, making it impossible to speak. However, if the patient is awake, they can communicate through gestures or writing.
Eating:
Also not possible by mouth while on a ventilator. Nutrition is provided through a feeding tube placed in the nose or directly into the stomach. This ensures the patient receives all essential nutrients.
Does the Patient Feel Pain on a Ventilator?
The ventilator itself doesn’t cause pain. What causes discomfort is the presence of a foreign tube in the airway.
To manage this:
-
Patients are initially sedated
-
Over time, they get used to the tube
-
Medical staff constantly monitor for signs of pain or discomfort and address them promptly
How Long Can a Patient Stay on a Ventilator?
There is no fixed timeline.
Duration Depends On:
-
The nature of the illness
-
The patient’s age and strength
-
The speed of recovery
Some patients may need ventilator support for a day or two, while others may remain on it for weeks or longer.
In rare cases where long-term ventilator support is needed, doctors may recommend a tracheostomy – a small surgical hole in the neck for easier and safer breathing support.
What Do Ventilator Readings Mean?
Ventilators have complex settings, but families can understand two key parameters:
1. Oxygen Percentage (FiO2)
This shows how much oxygen is being delivered. Normal air has 21% oxygen. On a ventilator, this can be increased up to 100% if needed.
2. Breathing Support Level
This refers to whether the patient is breathing on their own with some help or if the ventilator is doing all the work.
How Do Doctors Wean a Patient Off a Ventilator?
Weaning means gradually reducing ventilator support as the patient improves.
Steps Involved:
-
Improvement in Illness: The root cause (e.g., infection or trauma) must be under control.
-
Breathing on Own: The patient should begin breathing partially on their own.
-
Monitoring: Doctors monitor oxygen levels, BP, heart rate, and breathing capacity.
-
Extubation: If all signs are stable, the tube is removed, and the patient breathes independently.
If the patient cannot breathe well after extubation, they may be placed back on the ventilator temporarily or advised a tracheostomy if needed.
Can a Patient Be Kept on a Ventilator Indefinitely?
In some complex medical cases, yes.
Patients with chronic lung diseases, spinal cord injuries, or neurological conditions may require prolonged ventilator support. In such situations:
-
A tracheostomy is usually performed
-
The patient may be moved to a long-term care facility
-
Ventilation may even continue at home with the help of a portable ventilator
Important Facts Families Should Know

1. The Patient Is Alive on a Ventilator
Even if the patient isn’t moving or responding, as long as vital signs like heart rate, blood pressure, and brain activity are present, they are alive.
2. Patients Can Recover
Don’t lose hope. Many patients leave the ICU after ventilator use and go on to live healthy lives.
3. Doctors Always Aim to Wean Patients Off
No doctor wants a patient to remain dependent on a ventilator. As soon as it’s safe, doctors initiate weaning protocols.
Final Thoughts
Ventilators are life-saving devices used only in serious medical situations. They are not a tool for profit, nor are they a sign that all hope is lost. Understanding their purpose, function, and role in recovery can help families support their loved ones with clarity and confidence.
Key Takeaways:
-
Ventilators assist patients who cannot breathe on their own
-
They are used only when medically necessary
-
Patients can and do recover from ventilator support
-
Sedation is used to ensure comfort
-
Speaking and eating aren’t possible while intubated
-
Doctors carefully monitor and try to wean patients off as soon as possible
If you or someone you know is facing this situation, don’t hesitate to ask the medical team questions. Understanding the process makes it easier to face this difficult time with informed hope.